Archive for January, 2010
Posted on January 29, 2010. Filed under: News stories, Polyclinics, Providers | Tags: The Practice |
Pulse | By Steve Nowottny | 29 January 2010
The founder of a private provider running a series of GP practices across the country has issued a public plea to the Conservative party to maintain the ‘momentum’ of the polyclinic rollout if they win the general election.
Dr Jeremy Rose, clinical director and founder GP of The Practice, which currently runs nine GP practices and four GP-led health centres, and plans to open a further four shortly, also urged the Conservatives to bring in more private providers to help drive up health outcomes.
Writing in the Times, Dr Rose argued that polyclinics had helped shift care to the community and improve patient choice.
‘With a change in government and policy, momentum will inevitably be lost,’ he wrote. ‘Many of the reforms in the manifesto are not new, but combined and introduced in a sustained way, they could effect change in the NHS.’
‘Facilitated by the polyclinic concept with an array of GP services, outpatient clinics, health information and so on in one place, the number of clinicians a patient needs to see and the number of clinics they attend is reduced, thus speeding up the process.’
He added: ‘As the NHS has evolved over recent years the presence of independent organisations has increased and a notion of payment by results is becoming more widely accepted. At the core is a drive for clinicians to achieve the best health outcomes for everyone, wherever they live.’
‘The possibility of more independent providers could be a catalyst for just this.’
Pulse reported earlier this month that the Conservatives have opened up talks with a series of private providers after pledging to step up the role of the independent sector in the NHS. The party said talks were ongoing with ‘a wide range’ of providers from the private and voluntary sectors.
Read Full Post |
Make a Comment ( None so far )
Posted on January 28, 2010. Filed under: GP-led health centres, News stories, Providers | Tags: Out-of-hours, The Practice |
Pulse | By Gareth Iacobucci | 28 January 2010
Private firms will be able to cover extended-hours shifts for practices that do not to provide the service, under the next stage of the Government’s controversial drive to widen access to primary care.
Neighbouring practices could also take on the shifts, in a move the GPC has denounced as ‘a terrific recipe for fragmenting care’.
A letter sent to PCTs and SHAs by Gary Belfield, DH head of primary care, sets out how the Government plans to implement prime minister Gordon Brown’s pledge that all patients would have access to evening and weekend appointments.
The letter, providing details on the extension of the extended hours DES for 2010/11, makes clear that practices will not be forced to offer extended opening themselves, but that other providers will be drafted in where a practice does not.
It says: ‘A key priority is to seek to provide access to evening/weekend appointments for patients whose practices are not providing extended opening, for instance by asking other practices to provide this services, or by commissioning out-of-hours providers to offer bookable appointment slots for routine care.’
One firm, the Practice PLC, which has won a string of GP-led health centre contracts, has already indicated its willingness to take on extended-hours shifts.
Dr Jeremy Rose, clinical director and founder GP of The Practice, said: ‘The Government’s proposal is something we support and is a principle already being delivered at GP-led health centres to non-registered patients. The traditional view patients value continuity of care more than convenience is becoming questionable.’
Latest figures show around 77% of practices offering extended hours, but the Government wants access for all patients and has agreed PCTs should plough £161m into commissioning extended opening 2010/11 under the updated DES.
But GPC chair Dr Laurence Buckman attacked the proposal, calling it ‘an aggressive act against general practice’.
‘Patients will be baffled by this, practices will be angered by it,’ he said. ‘It’s deliberately designed to antagonise practices who are not offering extended hours, and I’m not sure it will improve the care of those patients either.’
Read Full Post |
Make a Comment ( None so far )
Posted on January 27, 2010. Filed under: GP-led health centres, Press/News Releases, Providers | Tags: Foundation Trust, Harmoni, Out-of-hours, Thamesdoc |
Harmoni website | accessed 27 January 2010
Harmoni is delighted to announce that Thamesdoc GPs have voted unanimously in favour of their Board’s recommended merger with Harmoni.
Stephen Price, Chief Executive of Thamesdoc, said “The recent Care Quality Commission interim report highlights the importance of delivering a high quality service where patient care and patient experience are the top priority. We believe that this adds further weight to the move for Out of Hours providers to consolidate in order to have the scale to deliver the best patient care. Thamesdoc and Harmoni are a natural fit. We share common roots as GP based Co-Operatives, have a good fit culturally and are geographically adjacent. I am confident that this merger will enhance the ability of both organisations to deliver high quality care to the populations we serve”.
Andrew Gardner, Harmoni’s Chief Executive, said “This merger reinforces Harmoni’s position as the market leader in the provision of Urgent Care services in England, and further enhances our ability to invest in the people, infrastructure, systems and processes required to provide the best possible patient care. We will set up a new Region based on the South East Coast Strategic Health Authority geography made up of the two companies existing services in Surrey and West Sussex and targeting the new opportunities that are emerging across the rest of the SHA. We will retain the Thamesdoc brand in Surrey where it is well respected and continue to use the Harmoni brand elsewhere.””
Harmoni is a leading provider of primary care services to more than 6 million patients across England. Its services are commissioned by over 20 NHS PCTs and include Out of Hours services, GP led Health Centres, Urgent Care Centres, Single Points of Access and Admission Avoidance schemes.
Thamesdoc is a GP co-operative providing Out of Hours and other urgent care services to patients in Surrey and parts of West Sussex and Hampshire.
Read Full Post |
Make a Comment ( None so far )
Posted on January 27, 2010. Filed under: GP-led health centres, Press/News Releases |
NHS Harrow | News Release
Harness Harrow GP-led Health Centre, opens at 46 South Parade, Mollison Way, Edgware, HA8 5QL, on 11th January, and will be open 8am to 8pm, 365 days a year. The centre will have two GPs at all times, with seven GPs employed in all. Registered patients will be able to book appointments in advance or on the day, whilst they and unregistered patients will have the option of walking in without making an appointment. The new service will provide patients with more consultation time with GPs and nurses, as well as ECG scans and blood testing on site.
Dr Sarah Crowther, chief executive of NHS Harrow, said the centre would be part of a redeveloped health system in East Harrow: “I am delighted that the Harness Harrow GP-led Health Centre is open – it’s a centre that will provide more services than ever before in East Harrow, and it is shaped around the needs of local people. The idea that you can get a blood test or a scan at your local surgery is something we are keen to roll out across the borough to make life easier for Harrow residents. We would like this centre to be part of a wider polysystem in East Harrow, which will mean that everyone in the area could be sent to local centres by their GPs when they needs tests or scans rather than going to the hospital.”
The new centre has been welcomed by local councillors too, with Overview and Scrutiny Committee Chairman Cllr Stanley Sheinwald praising the decision to keep the surgery open: “When NHS Harrow first consulted with the Scrutiny Committee, we ensured we were given all the facts and we were very thorough in our recommendations. We made it clear to NHS Harrow that the preferred option for Queensbury residents would be to keep the Mollison Way Surgery open, and after due consideration, this has been achieved.”
Cllr Dinesh Solanki, whose Queensbury ward will be served by the Mollison Way Surgery, said: “We felt that NHS Harrow was very receptive to the concerns that we had heard from our residents and every avenue was explored before a decision was reached.”
He added: “I am very pleased with the results –we now have a practice that will be open from 8am to 8pm, seven days a week and will serve local residents better than ever. It is a particularly positive result for older residents and people with long-term conditions, as it brings more services closer to where people live.”
“Over the last 18 months, the Scrutiny Committee has worked really hard with the PCT on bringing this to fruition. We have also worked together on securing the specialist stroke and major trauma unit for Northwick Park Hospital, due to open in April 2010, and it’s great to see the that our hard work is paying off for local people and will make a lasting difference. We are proving that an open and honest partnership between NHS Harrow and Harrow Council brings the best results for all our residents.”
Read Full Post |
Make a Comment ( None so far )
Posted on January 27, 2010. Filed under: News stories | Tags: Out-of-hours |
Pulse | By Gareth Iacobucci | 27 January 2010
A leading defence body has warned that complaints against GPs related to out-of-hours consultations are growing in number, with a 50% increase seen in the past two years.
The Medical Defence Union said it had been notified of 517 complaints related to out-of-hours consultations by GP members in 2007 and 2008, compared to 337 in the previous two years, an increase of 53%.
The study follows renewed calls from the Conservatives for GPs to take back responsibility for out-of-hours care, and the on-going inquest into the death of a patient given a fatal overdose by out-of-hours German locum GP Dr Daniel Ubani.
The MDU’s study found that OOH complaints now represented around 10% of the annual total of GP complaints, compared to 8% in the previous two years.
In total, the MDU reported 73 claims related to OOH consultations over the two years of the study, compared to 41 in the previous two years.
It also said only two claims have been settled to date, and in the MDU’s experience, around two-thirds of claims are discontinued or unsuccessful.
Dr Stephen Green, head of risk management at the MDU, said: ‘OOH care continues to represent a significant and growing proportion of the complaints we see. This analysis also highlights the communication challenges associated with OOH consultations which may make a complaint more likely if something goes wrong, compared to consultations within surgery hours.
‘For example, OOH consultations are generally associated with high levels of stress and anxiety for patients and their families: there may have been a wait to be seen by a doctor they have never met before; and they may feel more vulnerable because it is the middle of the night.
He added: ‘We are advising OOH doctors to pay particular attention to the need for clear, unambiguous communication with patients and colleagues, including accurate and comprehensive note-taking and arranging follow-up if necessary.’
Shadow health Minister Mark Simmonds blamed the increase on the Government’s changes to the OOH system back in 2004.
He said: ‘I have no doubt that this increase in complaints is mainly down to Labour’s flawed changes to the GP out-of-hours system, which took responsibility for the service away from GPs and gave it to local bureaucrats.’
KEY FINDINGS IN THE MDU STUDY
– 120 complaints and 52 claims included allegations of apparent failures or delays in diagnosis or referral. Most common conditions involved were myocardial infarction, septicaemia and meningitis. While it is inevitable that diagnoses will occasionally be missed, the MDU advises doctors to undertake and document the patient’s history and examination, including relevant negative and positive findings.
– 75 complaints and 17 claims were made following the death of a patient. It is impossible to rule out a sudden deterioration in a patient’s condition but it is important to review any diagnosis if there is any change and explain to patients and careers what to do if the condition does not improve.
– 71 complaints included allegations of rudeness or that the doctor had an uncaring or off-hand manner. One case featured an allegation that the doctor was chewing gum during the home visit.
– Problems with telephone triage featured in 19 complaints. In one case, a GP assessed a patient with abdominal pain and prescribed medication without visiting the patient, who later developed appendicitis.
– 13 complaints and claims in the study were referred to the General Medical Council (GMC). Four followed the death of a patient; two were sexual allegations and the majority of the rest related to poor performance.
Source: The Medical Defence Union
Read Full Post |
Make a Comment ( None so far )
Posted on January 25, 2010. Filed under: News stories, Polyclinics |
Ilford Recorder | ZJAN SHIRINIAN | 25 January 2010
THE Redbridge health roadmap was torn apart by an angry councillor who warned the borough would be lumbered with five run down polyclinics if it pressed ahead with plans to build more of the super surgeries.
Fairlop Polyclinic is one of four new health centres set to be built over the next four years to go alongside the existing Loxford Polyclinic, Ilford Lane, Ilford.
But the centres – housing GPs and a host of other specialist health services – are sparking unease.
At a coffee morning hosted by campaign group Barkingside 21 on Thursday, residents had the chance to grill Rob Meaker, chief officer for the Fairlop Polysystem, and Adrienne Noon, head of communications and marketing for NHS Redbridge.
In an angry outburst, Conservative Cllr Loraine Sladden – who was at the meeting in Fullwell Cross Library, High Street, Barkingside – warned building more polyclinics would be a mistake.
She said: “If you’re hell bent on polyclinics, at least get Loxford right first of all.
“A good business wouldn’t open another company if they have problems with the first one.
“Do it over three years and then come back if it works.
“Otherwise we will be left with five run-down polyclinics.”
Mrs Noon said: “Loxford has teething problems like any new entity.
“There are issues with the walk-in side of things and we are addressing those.”
She also told residents Fairlop Polyclinic, which would also serve Fullwell, Barkingside, Clayhall and Hainault, would be unable to house every health service, meaning some may have to travel further for medical care.
She said: “What we’re trying to do is say if there is a prevalence for this thing or that, lets provide for that in the closest polyclinic.”
She also denied suggestions doctors would be forced to close and move into the new super surgery.
The proposed closure of King George Hospital’s A&E was another topic at the meeting.
People raised concerns about the “complexity” of the public consultation’s questions and appointment waiting times.
Read Full Post |
Make a Comment ( None so far )
Posted on January 22, 2010. Filed under: GP-led health centres, News stories | Tags: Assura |
HEALTHCARE in Kingstanding has been given a boost after a doctors’ partnership signed up to run a new GP practice.
The new practice, based at the Warren Farm Health Centre, will be served by doctors from Assura Vertis, a group of 23 GP practices based in the Redditch and Bromsgrove area.
National investment has been provided to an area which has suffered a greater level of ill health and had access to a lower number of GPs than elsewhere in the country.
Jonathan Tringham, NHS Birmingham East and North director of resources, said: “I am delighted we are working in partnership to produce a new GP practice with high-quality services for patients.
“We have taken into account what our patients wanted from a GP practice and have incorporated views put forward through the public consultation.”
The initiative in Warren Farm Road follows extra funding as part of the Government’s Equitable Access to Primary Medical Care programme, which has enabled NHS Birmingham East and North to commission the new GP-led health centre.
The Warren Farm practice will work with the local community to develop an increased range of health facilities relevant to the local community and will provide extended access to health advice until 8pm two days a week and also on Saturday mornings.
Dr Ian Morrey, a local GP and Assura chairman, said: “We are pleased to have this opportunity to work with NHS Birmingham East and North to provide this additional access to a GP or nurse for the local community.
“We look forward to providing the patients of Kingstanding with high-quality, easy and convenient access to a GP or nurse.”
Read Full Post |
Make a Comment ( None so far )
Posted on January 22, 2010. Filed under: News stories | Tags: APMS, Provider-commissioner |
Pulse | By Yvette Martyn | NHS South West Essex | 22 January 2010
A PCT has announced plans to farm out 10 GP practices under a new wave of APMS tenders, in a move raising questions over the Government’s new-found commitment to ensure the NHS is the ‘preferred provider’.
NHS South West Essex will tender the contracts for the practices, which it currently runs, over the next 18 months as part of the process of splitting commissioning and providing roles.
Private companies and social enterprises will be allowed to bid for the contracts, even though health secretary Andy Burnham recently said alternative providers should only be sought to run services as a last resort.
In a sign of the confusion within Government policy, the PCT said the tenders were going ahead to satisfy a parallel drive to ensure PCTs only managed practices directly for short periods or in emergencies.
The first phase of tenders will see three practices transferring management with contracts to be awarded in Autumn 2010 and the remaining seven tenders to follow.
The trust insisted the move would not affect the services available or put the jobs of staff at risk. It said patients would be involved in the process and invited to give feedback on the plans, with a representative having input in the selection process.
Marc Davis, director of primary care for NHS South West Essex, says: ‘There are no plans to close or move any of the 10 GP surgeries, or reduce the range of NHS services available. The practices will still be NHS services, but like most other practices they’ll be managed by an independent contractor appointed by us.’
Dr Brian Balmer, chief executive of Essex LMCs, said: ‘The PCT has encouraged the GPs to bid for them and we are hopeful current employees will have a fair chance of getting a contract. We have organised training for GPs and practice managers in tendering and winning tenders.’
Read Full Post |
Make a Comment ( None so far )
Posted on January 22, 2010. Filed under: News stories | Tags: Out-of-hours |
Pulse | By Gareth Iacobucci | 22 January 2010
PCTs and out-of-hours providers who fall short of national benchmarking standards are to be named and shamed under new plans to drive up standards of care.
The Primary Care Foundation is planning to publish names of trusts and out-of-hours providers, and patient feedback, as part of the next phase of its NHS-funded national benchmarking scheme.
The plan is outlined in the group’s latest report, which analyses the lessons learned from the first phases of its benchmarking scheme.
It comes as the inquest into the death of a patient given a fatal overdose by German locum GP Dr Daniel Ubani has prompted renewed calls from the Conservatives for GPs to take back ‘collective responsibility’ for out-of-hours care.
Although benchmarking information has so far been anonymised, it has exposed huge variations in the cost and quality of out-of-hours services.
The latest report warns many providers are missing ‘potentially urgent’ cases and suggests there is an ‘adverse impact’ where out-of-hours services are split between providers: ‘The next benchmark, planned for mid 2010, we expect to be open rather than anonymous. We are confident greater openness will help both commissioners and providers improve their services.’
Henry Clay, director of the Primary Care Foundation, said: ‘[At the moment] you have a PCT and provider doing X, Y and Z but can’t tell who they are. That feels daft.’
GPC chair Dr Laurence Buckman warned the mounting criticism over out-of-hours did not mean GPs should take back responsibility for cover, saying that would be ‘dangerous to patients’.
‘The BMA wants to see PCTs commission out-of-hours care with the involvement of local GPs. There also needs to be better investment and more rigorous monitoring, but there must not be a return to the system we had before the new contract.’
‘That would just mean replacing the current, poor system with a potentially dangerous one.’
Read Full Post |
Make a Comment ( None so far )
Posted on January 21, 2010. Filed under: News stories | Tags: Commissioning |
Health Service Journal | 21 JANUARY 2010 | BY NICK GOLDING
Primary care trusts should be “released” from commissioning acute care and left to concentrate on improving primary and community services, MPs have been told.
York University professor of health economics Andrew Street suggested that the Department of Health should fund hospitals directly, as part of his evidence to the Commons health select committee inquiry into commissioning last Thursday.
He said it was “difficult” for PCTs to control costs, a task made harder since the introduction of the payment by results tariff system.
Professor Street warned: “They are at financial risk.”
In his written evidence he said: “Either PCTs should be given the means to negotiate on an equal basis with hospitals or – more radically – they should be released from having to deal with hospitals altogether.”
He told the MPs: “This role could be undertaken centrally and PCTs would focus on the more neglected areas of primary and community care where there’s a considerable need for action.”
His written evidence added: “The transfer of responsibility would allow the DH to sharpen the incentives of payment by results, using the tariff more effectively to control volume, and it would better facilitate free patient choice of hospital.
PCTs that successfully kept patients out of hospital would receive a proportionately larger budget from primary and community care, he suggested, with the proportion increasing over time if strategies to reduce referrals proved successful.
But NHS North Yorkshire and York director of public health Peter Brambleby told the committee that he disagreed with the proposal.
“It’s important that someone is tasked with ensuring that the deployment of resources for that community genuinely reflects its needs,” Dr Brambleby said.
PCT Network director David Stout told HSJ commissioning was about improving patient pathways, not simply about payments between different organisations.
He said there were numerous attempts to invest in community based services, including community matrons and telemedicine to reduce the length of hospital stays or avoid unnecessary admissions.
However, he admitted PCTs had struggled to reduce acute activity and would need to do so in order to invest in community based services in the leaner years of public spending to come.
“The DH would have less means of influencing acute demand than PCTs,” he said.
Westminster PCT chief executive Michael Scott also disagreed with Professor Street’s proposal. “Controlling acute activity is undoubtedly challenging. But this isn’t the answer.
“The answer is to aggregate the scale to get the leverage you need.”
Mr Scott heads the North West London commissioning partnership, which aggregates commissioning across eight PCTs, with an acute commissioning budget of £1.4bn.
He said Professor Street was proposing the “ultimate aggregation” by centralising all of acute commissioning, but that took aggregation too far.
“You would lose local control and flavour and you wouldn’t be able to incentivise shifting care from the acute to community sector,” he said.
Read Full Post |
Make a Comment ( 1 so far )
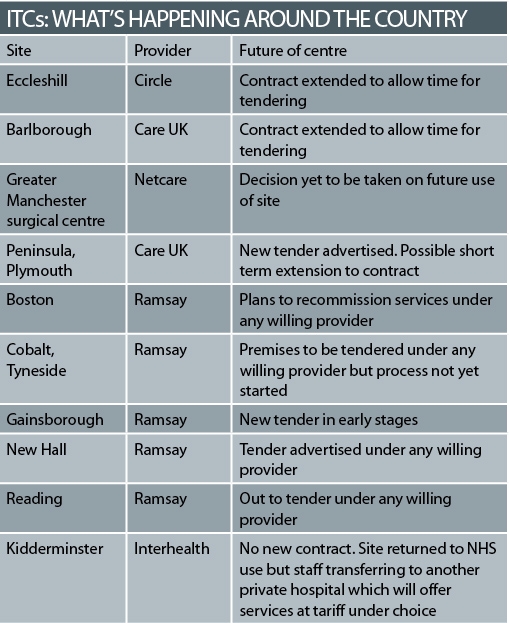
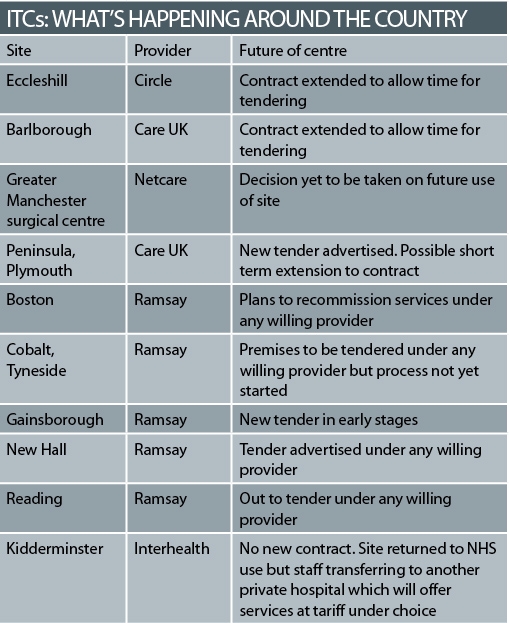
Posted on January 21, 2010. Filed under: ISTC, News stories, Providers | Tags: Care UK, Circle, Interhealth, Netcare, Ramsay |
Health Service Journal | 21 JANUARY 2010 | BY ALISON MOORE
The process for renewing contracts for the first independent treatment centres has been described as a “pig’s ear” by the chief executive of the largest independent provider in that sector.
Ten of the “first wave” contracts are due to expire in the next six months – with the general election expected midway through that period – and the future of many of the centres is uncertain.
At least one, the Kidderminster treatment centre in Worcestershire, is likely to close its doors. The centre will return to NHS use from next month, although the team running it plans to continue doing NHS work at a local independent hospital.
The future of the Greater Manchester surgical centre hangs on whether owner Trafford Healthcare Trust decides to use the site itself or to rent it out.
Many of the others are likely to continue but will offer treatment at tariff through patient choice, rather than through a block contract.
The firms running the centres have been told they have to go through a tender process to rent the buildings from the NHS – leading to uncertainty for staff and patients.
Mike Parish, chief executive of Care UK, which operates two sites coming up for renewal, said this had led to a “pig’s ear of a process”, with firms being offered short term contract extensions at the last minute because primary care trusts still had the contracts out to tender.
At the Barlborough centre in Chesterfield, run by Care UK, staff had to be formally told they were at risk of redundancy – only for managers to hear the next day that its contract had been extended.
“We have gone absolutely to the precipice with Barlborough,” said Mr Parish. “We have now agreed a short term tenancy with the PCT to give them an extra three or six months to sort out the lease.”
Several PCTs are at an early stage in inviting tenders for their sites. Lincolnshire PCT does not expect a new contract to come into force at its Gainsborough site until next year, according to tender documents. Many new leases will be for only three years, so PCTs and centre operators may have to repeat the process in 2013.
Mr Parish said independent centre operators had expected to switch to payment at tariff for any patients they could attract at the end of the original five year contracts, which offered guaranteed payments regardless of the number of patients treated.
But they learnt a few months ago that if their premises were owned by the NHS, as most are, they would have to go through a tendering process in order to continue to use them. Operators will pay market rent for the sites in future.
“The Department of Health, in its wisdom, decided that there would be some sort of procurement process for the leases,” he said. “It does seem odd that we have to go through a tender process to continue operating hospitals that we have operated for the last five years while NHS hospitals don’t.”
Care UK hit the headlines last week after reports its chairman had made a £21,000 donation to shadow health secretary Andrew Lansley’s office.
Health secretary Andy Burnham wrote to Mr Lansley questioning whether it was acceptable for a shadow minister
to “accept private donations from companies that have a vested interest in their policy areas”.
A Conservative spokesman said the donation was “fully within the rules”.
Independent provider Ramsay said it “understands the need” for a tendering process but some contracts may have extensions to allow this to be concluded.
The Department of Health said it announced in July that there would be a competitive tendering process where the NHS had identified a continuing need for services. It added there has been “an ongoing dialogue” between providers, the local NHS and the DH in each area.
Care UK and Ramsay may apply to run centres they do not operate at present, and Netcare – which runs the Greater Manchester centre – says it will consider case-by-case bidding.
NHS Partners Network director David Worskett was critical of the delay in resolving the contracts.
In some cases, operators will be paid at tariff but are being given “activity plans” by PCTs – an indication of the level of work they will be doing, which should help manage cash flow.
In others, PCTs say they now have sufficient capacity in the local healthcare system but they are willing to lease premises if the independent contractors take the risk of attracting sufficient patients.
The centres will also no longer be bound by “additionality” rules, which prevented NHS clinicians working in them and often forced them to recruit clinical staff from abroad.
Read Full Post |
Make a Comment ( 1 so far )
Posted on January 20, 2010. Filed under: GP-led health centres, Press/News Releases | Tags: Hurley Group, Walk in centre |
NHS Lewisham
NHS Lewisham (Lewisham Primary Care Trust) is delighted to announce that the Hurley Group has been selected as the preferred provider to deliver primary care services for the new GP Led Health Centre and Walk in service at the Waldron Health centre, Amersham Vale, SE14 6LD.
The Hurley Group have an excellent track record in delivering high quality GP led, patient centred healthcare for the NHS. They currently run one of the first GP led Walk in Centres that opened in London, based at the Lister Health Centre in Southwark and have successfully delivered services in a number of challenging South London environments.
Situated directly opposite New Cross railway station just off New Cross Road, the GP led Health Centre will deliver services to patients whether they are registered or non-registered (walk in) at the Centre.
The new service will improve access to healthcare in the area, offering extended opening hours and access to a GP between 8am to 8pm, seven days a week, 365 days of the year. It will offer bookable and non-bookable (open access or walk-in) appointments. The new service is expected to open in March 2010, when the existing nurse led walk-in centre at Goodwood Road moves to the purpose built primary care centre at the Waldron and services transfer.
The additional enhanced service offered by the GP led Health Centre complements the existing services provided by the 4 Doctors surgeries currently in the Waldron Health Centre. This will improve access to local people, walk-in patients and commuters. The Waldron Health Centre already houses a wide range of services under one roof including midwives, phlebotomy, foot health clinics, sexual and reproductive health, speech & language therapy, and services such as child health clinics. Pharmacy and optician services will also be provided in the near future.
The Health Centre and Walk in service development is part a national programme for Equitable Access, supported by the Department of Health, in response to public consultations (where access was a significant issue for a large number of patients). In addition NHS Lewisham have broader plans to develop the Waldron Health Centre by providing a range of services often associated more closely with hospital care. This is part of their drive to deliver care closer to home, improve health and well being and reduce health inequalities.
The Hurley Group is delighted to have been awarded preferred provider status. Dr Mark Ashworth, Organisational Medical Director, said:
“This represents a milestone for the Hurley group – we can combine our clinical knowledge, with our experience of delivering high quality care, in a state of the art purpose built facility. We are extremely pleased to have been selected to run the GP Led Health Centre in Lewisham especially as this is an area where we feel we can contribute to the wider local community.”
Who to contact about this article
Name: Matt Adcock
Email: matthew.adcock@lewishampct.nhs.uk
Telephone: 020 7206 3333
Fax: 020 7206 3338
Organisation: NHS Lewisham
Address: Cantilever House, SE12 8RN
Read Full Post |
Make a Comment ( None so far )
Posted on January 19, 2010. Filed under: News stories | Tags: Competition |
Pulse | By Gareth Iacobucci | 19 January 2010
The Department of Health has become embroiled in a row over a GP practice’s plans to open a branch surgery, after a PCT refused to allow the development to proceed, despite the Co-operation and Competition Panel (CCP) ruling in the practice’s favour.
The panel last month ruled in favour of Churchill Medical Centre after concluding that NHS Kingston’s decision to prevent the practice from expanding nearby was ‘inconsistent’ with competition rules.
But the PCT has refused to give permission for the practice to open its branch surgery until they are given directions by either the Department of Health or NHS London.
The competition panel has no legal power, but was set up by the Government to rule on cases where the Principles and Rules for Co-operation and Competition were in danger of being breached.
In December, it concluded that the PCT’s decision to deny the opening of a branch surgery was anti-competitive and restrictive to patient choice.
But in a letter to the practice, seen by Pulse, David Smith, chief executive of the PCT said: ‘The CCP report makes recommendations to the Department of Health and to NHS London regarding the branch surgery. Until such time as the DH and NHS London has considered the report, we will not give you permission to open the branch surgery.’
Dr Charles Alessi, a GP at the Churchill Medical Centre, said he was bemused that the PCT was still unwilling to allow them to open the branch surgery, despite the panel’s recommendation.
He said: ‘The competition panel can’t force [a decision], but it has been set up by the Secretary of State so one would assume that if they have found that the actions of the PCT breached elements of competition, the PCT take note of that.’
‘We are in a rather odd situation. We have contacted the DH and we are told that there will be some determination over the next few weeks. But there is a concern that the determination may include looking at the case yet again.
Dr Alessi said he hoped the DH’s determination would draw a line under the case, to allow them to provide a better service for their patients.
‘The whole basis of the competition panel’s verdict is that potentially our population is being denied choice and is being disadvantaged. That is being allowed to continue. One would hope the DH issue an instruction and we move on.’
Read Full Post |
Make a Comment ( None so far )
Posted on January 19, 2010. Filed under: News stories | Tags: Out-of-hours |
Pulse | By Steve Nowottny | 19 January 2010
GPC chair Dr Laurence Buckman has issued a robust response to mounting criticism over out-of-hours care, warning that giving back personal responsibility for its delivery to GPs would be ‘dangerous to patients.’
An inquest into the death of a patient given a fatal overdose by German locum GP Dr Daniel Ubani has prompted a storm of negative coverage in recent days, with two highly critical columns in the Independent and in the Times, and renewed calls from Conservative health spokesman Andrew Lansley for GPs to be ‘collectively responsible’ for out-of-hours care.
Independent columnist Mary Dejevsky chided GPs for working ‘office hours’, and questioned whether ‘those who effectively clock on at 9am and off at 5pm really deserve the status the rest of us reserve for committed professionals.’
‘It is surely no coincidence that as GPs have fled out-of-hours working, more and more people have resorted to A&E departments,’ she wrote on Friday. ‘If the NHS wants to improve A&E, it should start by demanding more of GPs.’
But in a letter to the Times, which has yet to be published, and the Independent, published today, Dr Buckman insisted he had ‘never worked a 9-5 day’ and strongly defended the decision of most GPs to opt out of responsibility for out-of-care.
‘The current out-of-hours sytem desperately needs improving, but we can’t go back to where we were before 2004 where doctors were on call 24 hours a day, meaning many were operating in a constantly sleep-deprived state,’ he wrote.
‘We are where we are now with out-of-hours because right from the start of the new contract many primary care trusts were more concerned with cutting costs rather than ensuring patients go the best quality care.’
‘The BMA wants to see primary care trusts commission out-of-hours care with the involvement of local GPs. There also needs to be better investment and more rigorous monitoring, but there must not be a return to the system we had before the new contract.’
‘That would just mean replacing the current, poor system with a potentially dangerous one.’
In the wake of the Ubani case the Conservatives have reiterated their pledge to hand back overall responsibility for out-of-hours care to GPs.
Mr Lansley said: ‘When Labour took responsibility for out-of-hours care away from GPs they made a serious error.’
GPs ‘are best placed to ensure patients are treated properly and that these awful events are never repeated again,’ he added.
Dr Michael Dixon, chairman of the NHS Alliance, has also entered the fray, insisting that GPs are best placed to deliver OOH care.
‘Recent cases have highlighted the importance of local responsibility for out-of-hours services, ideally manned by local doctors and nurses, who are familiar with their communities and the services that support them,’ he said.
BUCKMAN’S LETTERS IN FULL
Letter to the Independent
Dear Sir or Madam,
Like everyone I have great sympathy for all those involved in the Ubani case and I agree with Mary Dejevsky that the current out-of-hours service for patients is nowhere near what it should be, but I am afraid she misses a vital point when she compares GPs to other professionals (Note to GPs: some jobs have to be 24/7, Friday 15 January 2010). As this case highlights, when doctors make mistakes the consequences can be tragic, and a tired doctor is a dangerous doctor.
The current out-of-hours system desperately needs improving, but we can’t go back to where we were before 2004 where doctors were on call 24 hours a day, meaning many were operating in a constantly sleep-deprived state. Ms Dejevsky’s suggestion that we work shifts is not an unreasonable one, but it would make it very difficult for our regular patients, such as the elderly and those with chronic conditions, to see the same GP twice. They tell us, time and time again, that they value continuity of care.
I am afraid I do have to take issue with Ms Dejevsky’s sweeping and unfair generalisation that all GPs work 9 – 5. I have never worked a 9 – 5 day in my surgery and I don’t know any other doctor who has either. All surgeries are open from 8am till 6.30pm, as a minimum, and I (like most GPs) am there from 8 to 8 doing things for patients.
We are where we are now with out-of-hours because right from the start of the new contract many primary care trusts were more concerned with cutting costs rather than ensuring patients got the best quality care. The BMA wants to see primary care trusts commission out-of-hours care with the involvement of local GPs, there also needs to be better investment and more rigorous monitoring, but there must not be a return to the system we had before the new contract. That would just mean replacing the current, poor system with an unsustainable, potentially dangerous one.
Yours faithfully,
Dr Laurence Buckman
Chairman of the BMA’s GPs Committee
BMA House
Letter to the Times
Dear Sir or Madam,
I understand why, as a patient, Libby Purves wants to see a return to ‘the good old days’ when, if you got ill, it was your family doctor who visited you in the early hours of the morning (If you must get ill, make sure it’s before 6pm, Monday 18 January 2010). I also agree that the current system needs changing, however, Ms Purves is viewing the past through rose-tinted glasses. For doctors, being on call twenty four hours a day, seven days a week took its toll; individual GPs were left permanently exhausted and the profession was facing a recruitment crisis. Those nearing retirement were getting out early and those looking to enter general practice were put off when they saw how burnt out they too would become. That is why most family doctors handed over responsibility for out-of-hours care when it was offered them; with the number of out-of-hours calls rising all the time they couldn’t physically do it any more.
The old system meant many doctors were tired and therefore potentially dangerous to patients and it is for that reason that the BMA, and the GPs it represents, would resist a return to doctors taking back personal responsibility for delivering care out-of-hours. However, some sort of middle ground needs to be reached as patients deserve better than they are getting now. The BMA wants to see primary care trusts commissioning out-of-hours care with the involvement of local GPs, better investment and a focus on more rigorous monitoring of out-of-hours services. But we can’t go back to a potentially dangerous old system which would, once again, have an impact on the quality of care patients receive in-hours and was therefore good for no-one.
Yours faithfully,
Dr Laurence Buckman,
Chairman of the BMA’s GPs Committee
British Medical Association
Read Full Post |
Make a Comment ( None so far )
Posted on January 19, 2010. Filed under: GP-led health centres, Press/News Releases, Providers | Tags: Malling Health |
NHS Kingston | Press Release | 19 January 2010
NHS Kingston has announced the preferred location of a new GP led health centre which will open later this year in Gosbury Hill, Hook.
The centre – the first of its kind in Kingston – will offer a range of walk-in services and appointments to both registered and non-registered patients.
The GP led health centre will operate in addition to Grays Medical Practice and Orchard Practice, which are already based on the site.
David Smith, chief executive for NHS Kingston, said: “It’s good news that a venue for the GP led centre has been found which will provide additional health services for local residents including walk-in services and longer opening hours.
“Patients who currently use the two GP practices on the same site can continue to have a relationship with their existing GPs – the new service is about providing additional health services for a wider patient group.”
At the end of last year, following an open tendering process, the Grays Medical Practice was appointed as the preferred bidder to buy the Gosbury Hill site and to develop new premises for both its own practice and the neighbouring Orchard Practice which occupies the same building.
The Grays Medical Practice will be leading the development of the premises which will include the new GP led centre. Malling Health will be contracted by NHS Kingston to run the GP led health centre and provide a high standard of service for local people.
Dr John Gray, from Grays Medical Practice, said: “We’re delighted to have the opportunity to take the Gosbury Hill site into the new decade for the benefit of all local residents. We’ll be using our expertise on local health needs to lead the development of the new premises.
Working with Malling Health and the neighbouring Orchard Practice, we’ll ensure there continues to be a high standard of health service for local residents.”
Plans are being developed for state-of-the-art premises that will be lighter, more spacious and enable the practices to benefit from the latest technological developments. A planning application is expected within the first few months of this year.
It is anticipated that walk-in services will be available at Gosbury Hill without impacting on current GP services. This will be achieved by some internal reorganisation of the building which is expected to be completed in April 2010.
In the longer term, the site will also provide additional health services for the local community as part of NHS Kingston’s ongoing polysystems programme bringing more services closer to home.
Notes to editors
What is a GP Led Health Centre?
In October 2007, Lord Darzi published the interim report of the NHS Next Stage Review (England only), which announced a number of immediate recommendations, including the establishment of 1 new GP-led health centre per PCT.
The GP Led Health Centre will be a new service that will offer GP and Nurse Appointments.
The centre will offer a full range of medical services to all registered and non registered patients offering pre-bookable appointments, walk-in services and other co-located services.
For more information on NHS Kingston’s polysystems programme go to www.kingston-polysystem.nhs.uk
For more information contact Sarah Campion, NHS Kingston communications team; tel:020
8339 8086, email: sarah.campion@kpct.nhs.uk
Read Full Post |
Make a Comment ( None so far )
Posted on January 18, 2010. Filed under: GP-led health centres, Press/News Releases, Providers | Tags: Assura |
Assura Group | Press Release | 18 January 2010
A new GP practice is set to open in north Birmingham following a contract award by NHS Birmingham East and North.
Operated by Assura Vertis LLP, the practice will be based at the Warren Farm Health Centre and will work with its local community to develop an increased range of health facilities relevant to the needs of the local population.
The practice will offer increased choice to local patients as well as extended opening hours by opening until 8pm two evenings a week and on Saturday mornings.
The contract was awarded as part of the Government’s national Equitable Access to Primary Medical Care (EAPMC) services programme which was designed to increase access to GPs in communities that have traditionally experienced greater levels of ill health and have access to a lower number of GPs than other areas.
Under the scheme NHS Birmingham East and North has been allocated extra funding to commission new GP practices and a new GP-led health centre. Following a detailed tender process, work on a new practice for Kingstanding was given the green light when the GPs came in to sign contracts with the trust.
Dr Ian Morrey, a local GP and chair of Assura Vertis, said: “Assura Vertis is pleased to have this opportunity to work with NHS Birmingham East and North to provide this additional access to a GP or nurse for the local community. We look forward to providing the patients of Kingstanding with high quality, easy and convenient access to a GP or nurse, when they need it.”
Director of resources for Birmingham East and North, Jonathan Tringham said: “I am delighted that we are working in partnership to produce a brand new GP practice with high quality services for patients. We have taken into account what our patients wanted from a GP practice and have incorporated views put forward through the public consultation.”
ENDS
Press enquiries regarding Assura Group to:
Andrew McKeon, AJM Public Relations.
Tel: 01423 734 560; Mobile: 07802 484 155
Louise Bathersby, Assura Group.
Tel: 020 7107 3830
Read Full Post |
Make a Comment ( None so far )
Posted on January 18, 2010. Filed under: News stories, Polyclinics |
East London Advertiser | 18 January 2010
RESIDENTS are being given the chance to voice their views on the future of health services in the East End at an NHS roadshow.
As part of the Health for North East London programme, services across the area are being transformed over the next 10 years which could see changes across seven primary care trusts, including Tower Hamlets.
And residents are being invited to four different locations from Thursday where NHS staff will be on-hand to give out information and answer any queries about the proposals.
Under the proposed changes, every patient in Tower Hamlets could soon have a ‘super health centre’, known as a polyclinic, on their doorstep where they could go for minor surgery or even give birth, rather than to their nearest hospital.
And the Royal London Hospital in Whitechapel would become one of only two major acute hospitals in the area.
The roadshow will be based at the London Muslim Centre in Whitechapel Road on Thursday from 10am-4pm, Tesco in Bromley-by-Bow on January 29 from 10am-4pm and Asda on the Isle of Dogs on Friday February 5 from 10am-7pm.
It will also be in the Royal London’s Outpatients Department on Wednesday February 10, from 9.30am-12.30pm.
Read Full Post |
Make a Comment ( None so far )
Posted on January 18, 2010. Filed under: News stories, Providers | Tags: Circle, Competition |
Pulse | By Gareth Iacobucci | 18 January 2010
The Liberal Democrats have joined the Tories in condemning health secretary Andy Burnham’s pledge to treat the NHS as the ‘preferred provider’.
Speaking at private firm Circle Health’s conference in Bath last week, Liberal Democrat health spokesman Norman Lamb said the move to give NHS providers at least two chances to improve before allowing alternative providers to run services would severely hamper attempts to ramp up productivity in the NHS.
Mr Lamb said providers should be judged on quality, not on their status, and accused Labour of being in the pockets of the unions.
The move aligns the Lib Dems with the Conservatives, who have vowed to open up the market to more providers if elected, and, as Pulse revealed last week, have already begun talks with a host of private firms.
Mr Lamb said: ‘I strongly disagree with the secretary of state’s provider pledge; it is a stitch up with the unions. It will set back the task of improving productivity; you need that challenge to existing providers.’
He added: ‘You need that insurgency [from new providers]. It’s never the traditional providers coming up with the innovative ideas. The test should be quality.’
Shadow health secretary Andrew Lansley, also speaking at the event, accused Labour of back-peddling on its reform agenda, but said his party would push ahead with stimulating competition.
He said: ‘Not only was wave 2 of ISTCs abandoned, but Andy Burnham’s pledge is being interpreted as abandonment of any willing provider. The reform process hasn’t been pursued, and isn’t coherent. I will pursue any willing provider. As far as we can we should create a level playing field, and realise the benefits of competition.’
The views of both opposition parties were backed by Ali Parsa, chief executive of Circle, who urged the next Government to lower the drawbridge to all potential market entrants, and not waste time protecting existing providers.
He said: ‘We have a fundamental challenge. We now have to focus relentlessly on improving quality while reducing cost. Do we gamble on incumbents to make these changes? I don’t think they will be successful.’
‘My appeal to politicians is to bring down the barriers to entry. Do not waste your time and energy backing the British Leylands of this world. Let the talent come through. We have wasted billions of pounds supporting incumbents. Create the policies that lower the barrier to entry. It costs us nothing.’
Read Full Post |
Make a Comment ( None so far )
Posted on January 15, 2010. Filed under: News stories | Tags: Out-of-hours |
Healthcare Republic | Prisca Middlemiss | 15 January 2010
Patients from practices not offering extended hours will be able to book evening and weekend appointments at neighbouring practices from April.
Alternatively they will be allowed to book routine appointments with their local out-of-hours service.
The two new schemes spearhead health ministers’ drive to increase the population able to access extended hours.
At the last count in July 2009, 77% of practices offered extended hours.
Gary Belfield, acting director of commissioning at the DoH, has told PCTs and SHAs they are expected to spend their full 2010/11 allocation of £161m on improving GP access.
‘We would expect PCTs in the first instance to seek to maximise the number of practices agreeing to provide the extended opening hours DES (or equivalent arrangements) in the run-up to 1 April 2010.’
Practices must sign up for the extended hours designated enhanced service (DES) early in the financial year so PCTs can plan how to spend their spare cash.
Practices already doing extended hours may be asked to open on more evening or weekend slots.
Dr Richard Vautrey, deputy chairman of the GPC, said ‘At a time when PCTs around the country are under severe financial pressure, I suspect that few will have the necessary resources to make either of these suggestions work.’
Dr Laurence Buckman, GPC chairman, said: ‘If the government wants to spend money it doesn’t have on something that a very small minority of patients say they want, but do not necessarily need, that is for it to decide.’
Read Full Post |
Make a Comment ( None so far )
Posted on January 15, 2010. Filed under: News stories | Tags: Care UK, Conservative |
Healthcare Republic | Neil Durham | 15 January 2010
The Tories are insisting ‘donations from private individuals in no way influence policy-making decisions’ after private health provider Care UK donated £21,000 to fund the personal office of shadow health secretary Andrew Lansley.
Healthcare Republic has reported that Care UK runs GP practices, out-of-hours centres, clinical assessment, treatment and support services and walk-in centres
The Daily Telegraph broke the story that John Nash, a private equity tycoon and the chairman of Care UK, made the donation in November. However, the Tories insist that the donation was from Mr Nash’s wife.
A spokesman for the Conservatives said: ‘We have been completely transparent about this donation. It has been properly registered with the parliamentary register as well as with the Electoral Commission and is therefore fully within the rules.
‘John Nash and his wife have a wide range of interests, of which Care UK is just one. The donation to support Mr Lansley’s office was made through Conservative central headquarters. Mr Lansley did not solicit this donation. Donations from private individuals in no way influence policy-making decisions.’
Read Full Post |
Make a Comment ( None so far )
« Previous Entries